PGT-A explained
DNA is a molecule that contains information (in the form of genes) on how each cell in the body should grow and function. DNA is wrapped up into structures called chromosomes that are present in every cell in the body. Humans usually have 23 pairs of chromosomes (22 autosomes plus 1 pair of sex chromosomes) in each cell of their body. Having extra or missing chromosomes (aneuploidy) can result in failure of an embryo to implant, miscarriage and conditions such as Down syndrome.
PGT-A (formerly called PGS) checks whether an embryo has the correct number of chromosomes. Embryos that have the correct number of chromosomes are called euploid and those that do not are called aneuploid.
One of the main reasons an embryo fails to implant or results in miscarriage is a genetic (chromosomal) abnormality. Furthermore, the risk of genetic abnormalities being present significantly increases with maternal age.
For example, Down’s syndrome (a disorder of chromosome 21) is more prevalent in babies born to older mothers.
However, performing PGT-A on embryos before implantation will increase your chances of and reduce your time to a successful pregnancy. Also, you’ll not have ‘wasted’ transfers with embryos that could never lead to a successful pregnancy. Further, PGT-A will reduce the risk of miscarriage, and reduce the risk of a child being born with a genetic abnormality.

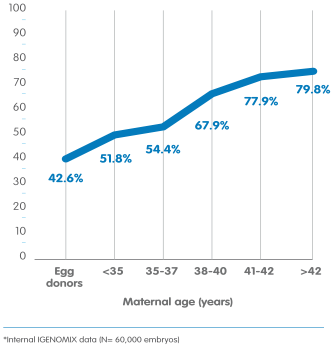
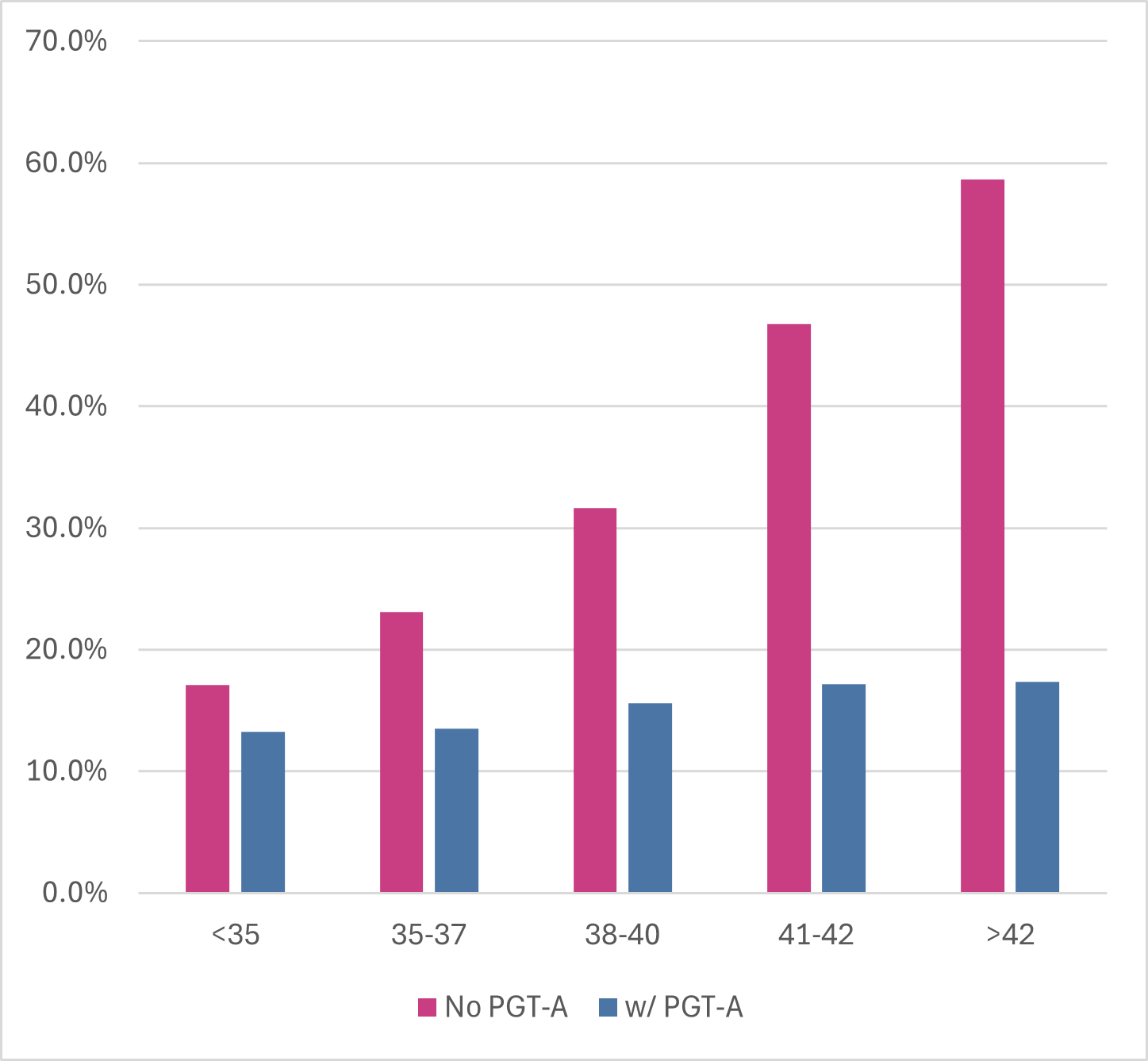
Risk of embryo damage by age
Here research shows the incidence of a aneuploidy (damaged) embryo with age
Currently PGT-A is a “treatment add-on” currently classified red by the HFEA owing to lack of an RCT for the effect of PGT-A on pregnancy and miscarriage rates. However, there was an RCT in women aged 38-41 that showed superior clinical outcomes in the PGT-A group: Rubio et al; Fertil Steril. 2017 May;107(5):1122-1129.
Research showing proven success
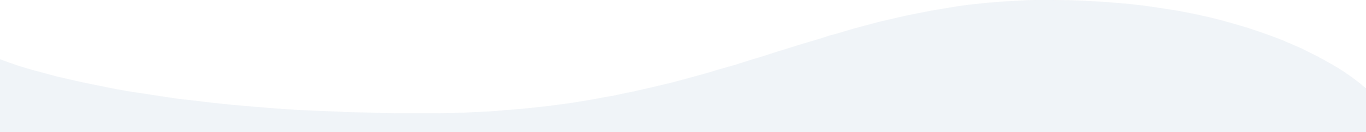
Increase your chances of a live birth with PGT-A


This compelling research proves that all age groups benefit from testing your embryo's with PGT-A in order to ensure the best quality blastocyst is implanted, and ultimately increased chance of a live birth.
Success in women over 40years triples!
Source: SART 2023
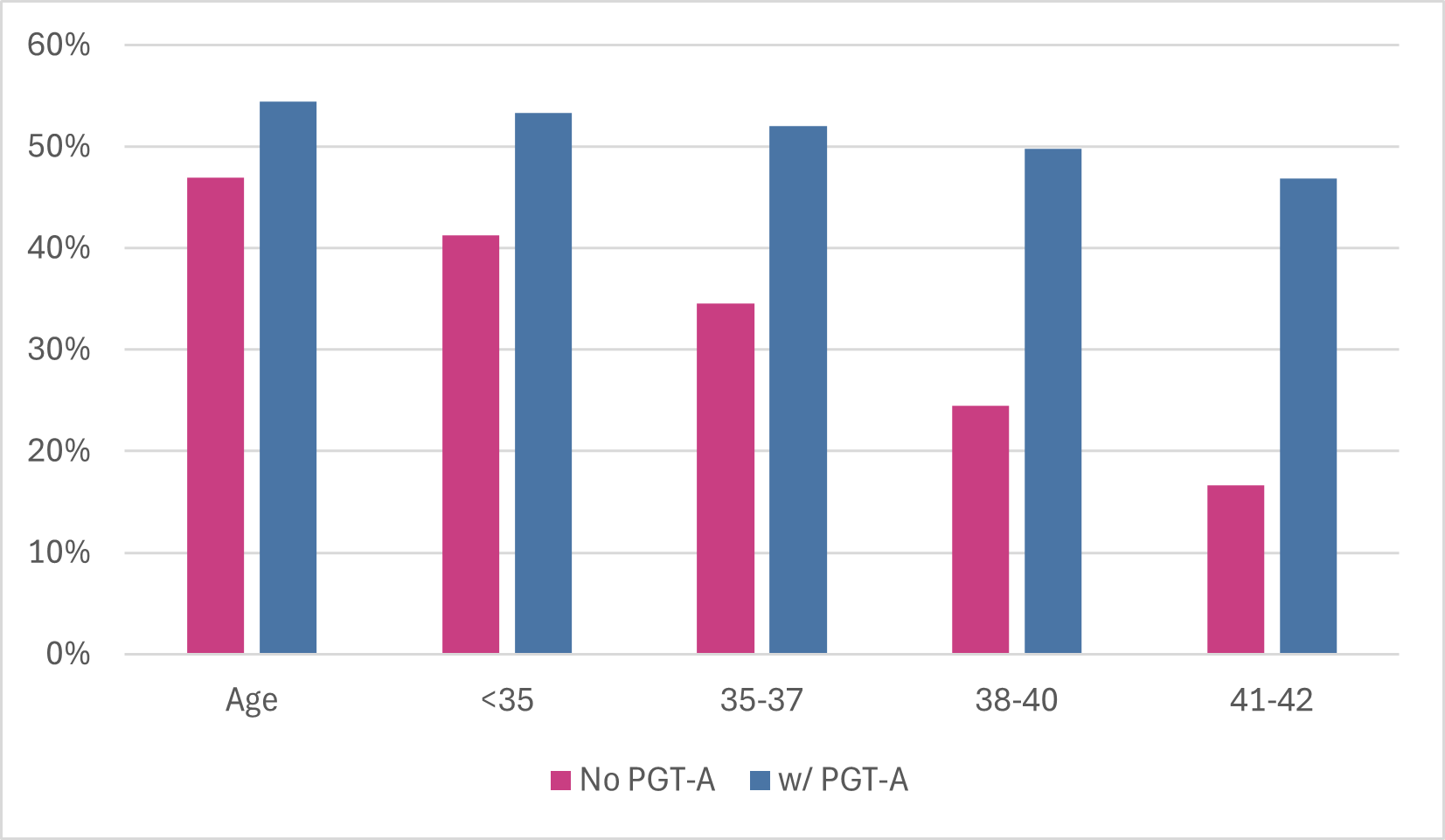
Gain confidence in PGT-A testing from the start of treatment.


Research shows that live birth rate doubles in success from each egg collection performed with mature women over 40 years. The results are still markedly improved with those in their thirties.
Source: SART 2023
Reduce risk of miscarriage with PGT-A test


Miscarriage can result from many factors. Early investigations before treatment can reduce those factors. PGT-A testing embryo's can avoid unnecessary miscarriage and heartache.
Source: SART 2023
PGT: what are the risks?
Genetic testing of embryos (PGT) is an invasive procedure so it’s important to understand the risks. Your doctor will always discuss everything with you, but we’ve also outlined what these risks are below.
Embryo biopsyThere’s no guarantee that embryos will be suitable for the biopsy procedure. If the biopsy does not take place, genetic testing cannot be performed. As with any invasive procedure, there is a risk of damage to the embryo from the biopsy procedure. However, it’s estimated that this risk is less than 1%.
Misdiagnosis
The risk of a clinical misdiagnosis resulting in a baby with genetic abnormalities after PGT procedure is less than 1%. This could be as a result of mosaicism within an embryo (cells with a different chromosomal pattern). If a pregnancy results, prenatal testing and/or diagnosis is advisable if your doctor recommends it.
No embryos for transfer
Genetic testing may reveal that all of the embryos are genetically abnormal, in which case there will be no embryo suitable for transfer into the uterus. The risk of this occurring is influenced by a variety of factors, the most important of which are family history, maternal age and the number of eggs retrieved.
No diagnosis
A small number of embryos may have no diagnosis due to poor DNA quality (often found in damaged or dying cells). Embryos without a result can still be transferred, but the benefits of genetic testing will not apply in such cases.
Gender selection explained
Gender selection is only allowed where there is a risk of having a child with a serious medical condition, and is strictly prohibited for social reasons e.g. to have a baby boy or girl to balance your family.
Some genetic diseases, such as Duchenne muscular dystrophy, are sex-linked disorders, which affect boys but not girls (girls may still ‘carry’ the gene for the disease but they will not suffer from it). In such cases the embryos are tested for their sex and only female embryos are transferred to the womb.